MHT
This portion of the OCJP Administrative Manual is provided for use by all subrecipient staff receiving state grant funds from the Office of Criminal Justice Programs for Mental Health Transportation projects. It is intended to serve as a reference for the programmatic requirements and responsibilities of projects funded through the Mental Health Transportation (MHT) Endowment Grant program.
Pursuant to Tennessee Code Annotated §33-6-406, “Subject to annual appropriations, there is established a grant program to assist sheriffs required to transport persons to a hospital or treatment resource for emergency mental health transport under this section. The Department of Finance and Administration, in consultation with the Department of Mental Health and Substance Abuse Services [TDMHSAS] and the Division of TennCare, shall develop and administer the grant program.”
Legislative Authority: Tennessee Code Annotated §33-6-406
1. The purpose of the MHT endowment grant is to help offset the costs of patient transportation for eligible subrecipients. Individuals who have never been arrested or charged with a crime are committed both voluntarily and involuntarily into state behavioral health hospitals on a daily basis across the State of Tennessee. While these individuals have not committed a crime, it is the responsibility of the local county Sheriff to transport this patient from the location where a certificate of need has been executed by a medical professional to the awaiting approved behavioral health facility.
2. Mental Health Transportation grants are provided as endowment grants with no pre-approved budget. Agencies submit the number of emergency mental health transports provided from the most recent previous fiscal year in which data is available. The grant funding available is subject to annual appropriation and the amount allocated is based upon a formula which uses eligible mental health transports across the state.
3. The Mental Health Transportation grant is limited to persons suffering from a mental health crisis, who have not committed a crime, should not be incarcerated, , or otherwise treated as a justice-involved individual accused of committing a crime. Since every case is unique, a one-size fits all approach is inappropriate, and deputies should have discretion on when to use restraints. Hospitals are preferred to jail cells, and unmarked vehicles are preferred to marked law enforcement vehicles. Persons suffering a mental health crisis are likely also experiencing trauma. Trauma Informed Care, Person-Centered care, and Recovery Oriented Care are all key concepts to a successful Mental Health Transportation program.
4. Assistance from this grant program must not be provided for emergency mental health transports where a physician, psychologist, or designated professional determines that the person can be transported by one (1) or more friends, neighbors, or other mental health professionals familiar with the person, relatives of the person, or a member of the clergy pursuant to §33-6-901.
5. A sheriff may contract with one (1) or more third parties or other law enforcement agencies to transport persons to a hospital or treatment resource in accordance with this section. The sheriff shall deem a third party or law enforcement agency contracted to perform this function to be the designated secondary transportation agent pursuant to §33-6-901. Any contract entered into is subject to audit by the comptroller of the treasury or the comptroller's designee.
6. A sheriff may receive grant funds provided under this subsection (c) and pay the grant funds to third parties or other law enforcement agencies with which the sheriff contracts to transport persons to a hospital or treatment resource in accordance with this section. The receipt or expenditure of grant funds received by a sheriff under this subsection (c) is subject to audit by the comptroller of the treasury or the comptroller's designee.
7. Key Definitions:
7.1. Person-centered – A philosophy that sees the people using health and social services as equal partners in planning, developing, and monitoring care to make sure it meets their needs. It involves putting people and their families at the center of decisions, seeing them as experts, and working alongside professionals to achieve the best outcome.
7.2. Recovery oriented – A practice acknowledging each individual is an expert on their own life and that recovery involves working in partnership with individuals and their caregivers to provide support in a way that makes sense to them.
7.3 Trauma informed care – A standard of care that understands and considers the pervasive nature of trauma and promotes environments of healing and recovery rather than practices and services that may inadvertently re-traumatize.
7.4. Trauma – Is an emotional response to a terrible event like an accident, rape, or natural disaster. Immediately after the event, shock and denial are typical. Longer term reactions include unpredictable emotions, flashbacks, strained relationships and even physical symptoms like headaches or nausea. While these feelings are normal, some people have difficulty moving on with their lives. (https://www.apa.org/topics/trauma, accessed 08/04/2021)
1. Eligible subrecipients are limited to: Sheriff’s offices or qualifying municipal governments in the state of Tennessee who conduct secondary transports as described under TCA § 33-6-406.
2. Sheriff’s offices may designate other entities, to include municipal law enforcement agencies or other third-party providers that meet the requirements for secondary transportation agents under TCA § 33-6-901 to provide the transportation on their behalf. Sheriff’s offices must first apply for this funding and then subcontract with other municipal law enforcement agencies or third-party providers.
3. If a municipal government designates an entity other than the sheriff as the provider of transportation as described under TCA § 33-6-406, the ordinance or charter that designates the secondary transport agent must be submitted with the application.
4. Patients vs. Inmates
4.1. The MHT grant is exclusively for expenses related to the transport of non-inmate patients. Individuals who are in the Sheriff’s custody for any charge, felony, or misdemeanor, who are not free on bond or Release on Recognizance bond, are ineligible to have their transport costs charged to this grant.
4.2. Agencies may have hospitals, emergency departments, or other medical providers who are unwilling to or state they are unable to hold a patient while a state hospital bed is pending. Sheriff’s offices are encouraged to reach out to the Tennessee Department of Mental Health and Substance Abuse Services, Office of Crisis and Suicide Prevention for assistance.
Agencies are required to:
1.1. Utilize unmarked vehicles for transporting patients
1.2. Wear soft uniforms while transporting patients. If a soft uniform is unavailable, the deputy may wear a plain jacket to cover their uniform shirt. No tactical uniforms or vets should be worn while transporting patients. Shirts and jackets may identify the deputy as law enforcement and have a badge embroidered on the shirt (as well as the deputy’s name if preferred).
1.3. Enact a Humane Transport Policy. (See subsection VII of this chapter).
1.4. Ensure staff are trained in behavioral health topics pursuant to the Humane Transport Policy
1.5. Ensure third party vendors have a valid Basic Life Support certification from the Tennessee Department of Health pursuant to the Rules of the State of Tennessee 1200-12-01-.14(3)(a)(2)(i); or otherwise meet the criteria listed in subsection XII.
1.6. Submit quarterly and annual reports.
1.7. Law enforcement agency must follow these requirements as well:
1.7.1. Fingerprint Reporting Requirement: The Agency shall ensure that they will comply with Tennessee Code Annotated (TCA) 38-3-122 and will submit all fingerprints to the Tennessee Bureau of Investigation (TBI).
1.7.2. Tennessee Incident Based Reporting System (TIBRS) Reporting Requirement: The Agency shall ensure that they comply with the rules and regulations of the TBI as empowered by Tennessee Code Annotated (TCA) 38-10-101 et seq. with regard to the TIBRS. The agency will at all times maintain TBI certification of their compliance with those rules and regulations.
1.7.3. National Instant Criminal Background Check System (NICS) Reporting Requirement: The Agency shall ensure that they comply with Tennessee Code Annotated (TCA) 33-3-1115 with regard to NICS Reporting. The agency will at all times maintain compliance.
1.7.4. Death in Custody Reporting Act (DICRA) Requirements: The Agency shall comply with PUBLIC LAW 113–242 by submitting all deaths in custody to the TBI.
1.7.5. Mandatory Reporting of Child Abuse and Adult Abuse: Agencies must comply with Tennessee Code Annotated, Sections 37-1-403 and 37-1-605 by reporting suspected cases of child abuse to the Department of Children's Services and with Tennessee Code Annotated 71-6-103 by reporting cases of adult abuse to the Department of Human Services as required by law.
1.8. Other requirements as listed in each fiscal year’s solicitation packet will be enforced. Agencies are encouraged to retain a copy of the official solicitation packet they download when applying for the grant.
2.1. All agencies participating in the MHT grant must implement a Humane Transport Policy. The purpose of a Humane Transport Policy is to guide the process of law enforcement mental health training, provide policy for humane transport for individuals in need of involuntary psychiatric hospitalization, and establish a standard for the least restrictive processes to be employed when transporting persons to mental health treatment facilities in a manner that does not criminalize, stigmatize, nor retraumatize those in need of care while ensuring the safety and security of all involved in the transport process. This policy is designed to address individuals who are not under arrest and are being transported pursuant to a certificate of need for emergency involuntary hospitalization issued in accordance with TCA § 33-6-404.
2.2. The OCJP in collaboration with the Tennessee Department of Mental Health and Substance Abuse Services, Division of TennCare, and Tennessee Sheriff’s Association developed a model policy that agencies may use to develop their own Humane Transport Policy. The model is available at: https://www.tn.gov/content/dam/tn/finance/ocjp/Humane%20Transport%20FINAL%201.22.21.pdf
3.1. The MHT program and Humane Transport policy require annual mental health awareness training. The training should provide information regarding principles and best practices for engaging and interaction with an individual subject prior to the individual’s first interview with a medical practitioner. Annual training should include an emphasis on expanding knowledge of trauma-informed care, verbal de-escalation, suicide prevention, medications, symptoms, developmental disabilities, and dementia.
3.2. There are multiple training programs and curriculums available that agencies may choose to implement that cover these areas. The following list of training programs and websites are provided to guide an agency towards an appropriate program; however, this list is not exhaustive.
Secondary Transport Agents (STA) refer to agents performing transports who are not sheriff’s employees.
4.1. Sheriff’s offices are free to subcontract or enter into a Letter of Agreement with a third-party vendor or secondary transport agent to subsume patient transportation on their behalf. The agent must meet one of the following criteria:
4.1.1. A valid Basic Life Support certification from the Tennessee Department of Health pursuant to The Rules of the State of Tennessee 1200-12-01-.14(3)(a)(2)(i); or
4.1.2. All STAs must meet the criteria listed in Tenn. Code Ann. § 33-6-901. Additionally, any subcontracts with a third-party agency that is not a law enforcement agency must include the following criteria:
4.1.2.1. STA requirements that must be addressed by subcontracts with a third-party agency:
a. STA services must be available 24 hours a day/7 days a week/365 days a year
b. All STA staff who interact with patients or protected health information (PHI) must successfully pass, before assignment, a state and federal background check, which must include, but is not limited to the following:
· Nationwide fingerprint criminal background check
· Tennessee Department of Health Abuse Registry check
· United States Department of Justice National Sex Offender Registry check
· Office of Inspector General’s List of Excluded Individuals and Entities (LEIE) check
c. In the event an STA staff is arrested, indicted, convicted, or issued a citation in lieu of arrest for a criminal offense, either a misdemeanor or felony, the STA staff member must immediately report this information to their direct supervisor within twenty-four (24) hours following the event.
d. If the direct supervisor is unavailable, the STA staff must report to the next supervisor or manager in the chain of command as appropriate. If the event occurs on a day the STA staff is not scheduled to work, it must be reported on the next workday.
e. All STA staff who interact with patients must successfully pass, before assignment, a 5-panel drug test. The five-panel drug test must test for the following substances:
· Amphetamines
· Cocaine
· Opiates
· Phencyclidine (PCP)
· Tetrahydrocannabinol (THC)
f. Have passed a physical examination by a licensed physician.
g. Have been certified by a Tennessee Licensed Health Care Provider qualified in the psychiatric or psychological fields as being free from any impairment, as set forth in the current edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM) of the American Psychiatric Association at the time of the examination, that would, in the professional judgment of the examiner, affect the person’s ability to perform an essential function of the job, with or without a reasonable accommodation.
h. All STA staff who interact with patients must maintain proof of completion of “Mental Health First Aid”.
i. All STA staff should ask the referring entity for relevant information regarding recent medications or treatments the patient has received that may impact transport.
j. Any STA drivers must maintain the following certifications:
· CPR/AED
· First Aid
· Emergency Oxygen Administration
k. Crisis Intervention Training (CIT) is highly recommended for all STA staff who would interact with patients.
l. “Handle with Care” Training is recommended for all transporting agents.
m. Drivers must maintain a valid driver’s license for the appropriate classification based on the type of vehicle and service provided.
n. An updated MVR for each STA driver must be obtained and reviewed by the STA throughout the duration of the driver’s employment with or by the STA.
4.1.2.2. STA vehicle requirements that must be addressed by subcontracts with a third-party agency:
a. Vehicles must be fitted with a driver-controlled door locking system so that the person in crisis is unable to open the doors of the vehicle without the assistance of the responders, reducing the risk of elopement.
b. Secure safety panels must be provided between the driver and passenger compartment. These panels should be transparent so that the driver can see behind to the passenger compartment.
c. Transport vehicles should also preserve the separation between the patient and the trunk space in the vehicle. In particular, if a transport vehicle is a van, a mesh or grille bulkhead should separate all equipment held in the trunk from the passenger.
d. Windows must be tinted for the privacy and dignity of the person being transported
e. Vehicles must be equipped with a portable AED (automated external defibrillator) and a first-aid kit. Other medical equipment should be made available as needed, i.e., oxygen tank and other supplies
f. Vehicles must have a lockable container to carry patient property.
g. The Patient area within the vehicle must be free from ligature risks or any items that may be used for self-harm.
h. As needed, STA vehicles must provide for the safety and adequacy of transport for those under the age of 18. As needed, this requires that STA vehicles be equipped with a booster seat.
i. For trips greater than 120 miles (or anticipated to exceed two (2) hours, STAs must allow stopping for restroom breaks for the patient at least every two (2) hours. For these transports, STAs must include two staff members, such that the personnel patient ratio is 2:1.
· STA staff must be prepared to be flexible if patient needs exceed this two-hour minimum.
· STA staff must be prepared to provide for the safety and security of each patient throughout the duration of the entire transport, to include, during any stops along the way.
j. Vehicles must be equipped with appropriate communication devices such that drivers can quickly access emergency assistance at any location within the state.
k. Devices must be hands-free in order to comply with all state laws.
4.1.2.3. Transport Ratios
STA may transport more than one patient at a time under the following circumstances:
a. A standard five-seat vehicle may transport no more than two (2) patients at a time.
b. A standard 10-passenger van may transport no more than four (4) patients at a time.
c. A minimum of two (2) staff persons must accompany the transport of a group of patients.
d. Transporting agent(s) should use judgment as it relates to the clinical profile of the patients they may be transporting together. Clinical judgment should also be consulted from the Emergency Department (ED) or the assessor.
4.1.2.4. Searching Patients
Patients must be searched prior to being transported to ensure they do not have anything that may be used to harm themselves or others. To do this safely:
a. The gender of the STA driver shall match the patient whenever possible.
b. The search shall be conducted with a witness observer or be recorded, preferably both.
c. STAs are encouraged to utilize a wand to assist in the search process.
Please note that pursuant to the Tennessee Department of Health as of August 2021, a secondary transport agent that is an ambulance service must have a BLS license in each county they wish to operate in. Questions about ambulance service requirements should be directed to the Tennessee Department of Health, Emergency Medical Services division at https://www.tn.gov/health/health-program-areas/health-professional-boards/ems-board.html.
1. MHT subrecipients must meet all allowable and unallowable cost requirements listed in the OCJP Grants Manual Chapter XIV. And XV. Moreover, the MHT grants are “endowment grants” with no specific budget being approved by OCJP. Agencies are provided their full grant amount shortly after the contract starts. Agencies are then free to allocate those funds for any reasonable, necessary, and allocable costs related to the transport of patients under TCA § 33-6-406.
2. Specific examples of allowable costs are provided below, but this list not exhaustive:
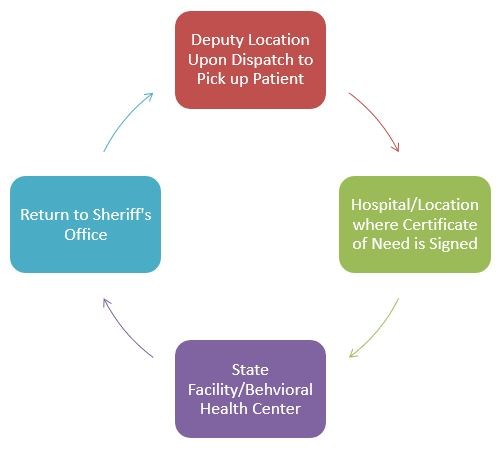
2.1 Mileage expenses – One full round trip from the Deputy’s dispatch location, through patient pick-up location (e.g., hospital), to patient drop off location (e.g., Middle Tennessee Mental Health Institute), and back to the dispatching Sheriff’s Office location. Mileage expenses may be charged to the grant at the current State Mileage rate published in the State of Tennessee Comprehensive Travel Regulations, F&A Policy 8.
2.2. Equipment – Agencies are free to purchase equipment with their MHT grant. This equipment should be used in the assistance of transporting patients. Equipment can include, but is not limited to:
2.2.1. Vehicles – sedans, vans, and SUVs are appropriate
2.2.2. Vehicle equipment such as metal/plexiglass barriers separating driver/passenger, barriers preventing unauthorized exit from patrol vehicle by patient, discrete code three lights, radios for vehicle including portable “check out” radio for MHT run, in-car video cameras, window tint, labor for installing equipment, GPS devices, transport seats, etc.
2.2.3. Soft Uniforms
2.2.4. Soft Restraints
2.2.5. First Aid Kits / AEDs
2.2.6. Safety Equipment – Equipment that helps an employee deescalate a situation and/or prevents injury to transporter or transportee in the event the patient is combative. Safety equipment can also include things like flashlights, BOLA wraps, soft restraints, etc.
2.2.7. Patient comfort measures, such as blankets.
2.3. Training – Mental Health / Behavioral Health awareness training that aligns with the Humane Transport Policy is an appropriate expense. This includes instructor fees, books/workbooks, training supplies, meeting space, and employee time/labor expenses to attend training. If overnight travel is required, the agency must follow the State of Tennessee Comprehensive Travel Regulations, F&A Policy 8.
2.4. Employee Time/Labor/Taxes/FICA and related expenses – Staff time, labor, and related expenses for performing duties related to MHT, including training, may be charged to the grant. Agencies should track employee time related to each transport and/or training sessions, preferably in a time keeping system.
2.5. For more information on allowable costs, please refer to chapter XIV of the Grants Manual.
3. Unallowable Costs are listed in Chapter XV of the Grants Manual.
3.1. There are no “pro-rating” requirements for MHT grant funds. Sheriffs Offices who buy vehicles for MHT may utilize the vehicle for other purposes as long as the vehicle is available for its primary purpose, Emergency Mental Health Transports.
The Project Director is responsible for timely submission of completed program reports each quarter and at the end of the year. Inability to submit required reports in a timely fashion is considered a failure of required contract obligations.
Time Frame |
Due Date |
July 1 – September 30 |
October 15 |
October 1 – December 31 |
January 15 |
January 1 – March 30 |
April 15 |
April 1 – June 30 |
July 31 |
Quarterly Mental Health Transport Tracking – This report is due quarterly per the table above:
This is a two-part report. The first part is a Formstack report, and the second part is a tracking spreadsheet which is uploaded via Formstack. The spreadsheet tracks the following data on two tabs.
1.1. Transport Records Tab:
1.1.1. Transport Date – Date the patient was transported either by Sheriff’s Office or third-party transport vendor under a certificate of need.
1.1.2. Agency Transport ID – The CAD number assigned to the event.
1.1.3. Starting Location – Pick up location of the patient, e.g., “Lake Parime Hospital, 123 Main Street, Nowhere, TN, 12345”.
1.1.4. Ending Location – Drop off location of the patient.
1.1.5. County – This column auto-fills from the first tab of the spreadsheet. Do not click here.
1.1.6. Validation – This column changes from Incomplete to Complete once sufficient information is entered in columns C – F.
1.2. Summary Sheet Tab: This tab functions as a validation check of sorts. There are only two cells on this page to change. County Name, which is a drop-down menu, and Quarter, which is also a drop-down menu.

The number of transports listed on the Summary Sheet tab is automatically summed from the Transport Records tab.
Mental Health Transport Year End Report – This report is due annually by July 31 of each year
For the MHT Year End Report, subrecipients must upload a reconciliation report to the Formstack.
This report totals up the amount of grant funds spent and is submitted online. The year-end report, also known as a reconciliation report, is emailed to the Program Manager in the final quarter of the fiscal year. The report is a simple excel spreadsheet with the following categories:
2.1. Equipment – Agencies should list each piece of equipment purchased, the date the item was purchased and received, and the purchase amount.
2.2. Mileage – Agency should total the number of miles driven to perform all transports and place on this tab. Mileage is paid at the prevailing state rate as published in Policy #8 of the Tennessee Department of Finance and Administration. Agencies may charge mileage from the deputy’s dispatch point, to the patient pick-up location, then to the patient drop-off location, and finally back to the Sheriff’s Office. Agencies are also welcomed to do a simplified mileage charge of one round trip from “hospital to hospital”.
2.3. Time and Labor – Agency should total all the hours worked on the grant and an average hourly rate (which may include insurance, FICA, taxes, etc.) and place on this tab.
2.4. Other Expenses – This should capture other expenses on the grant, such as third-party vendor transport costs, training expenses, etc. Please note the date the service or item was procured and the date the item was received, as well as the cost of the item or service.
2.5. Vehicles: This should capture a description of the purchased vehicle, the date it was purchased, the date it was received, and the total cost of the vehicle including any destination or dealer charges. Agencies can purchase either new or used vehicles.
2.6. Totals – This tab automatically sums all the categories together.
Every MHT contract must be monitored during the time the contract is active. Contracts are typically monitored in the spring of each year with contracts going live in the summer of each year. Monitoring is performed via a “desk review” where the grant’s project director shares key information with the OCJP Program Manager via a custom SharePoint folder. Items reviewed include:
Grant Folder and Contents |
Transports Are for Patients |
Spending Is Reasonable, Necessary, and Allocable |
Soft Uniforms |
Quarterly Reports on Time |
Comptroller Signage Posted |
Unmarked Cars |
Quarterly Reports Accurate |
Mental Health Awareness Training Completed |
Humane Transport Policy |
Documentation of Transports |
Subcontractors Meet Requirements |
Additional information about monitoring is available in Chapter XIX. Of the OCJP Grant’s Manual.